Weekly roundup
Here’s what you missed last week!
🏛️ Policy & Payers
Budget for a 6.5% benefits cost jump in 2026, the highest since 2010, per a national benefits survey.
Fewer hoops if you perform: UnitedHealthcare’s gold card program expanded 40% in 2025 to cut prior auth for compliant groups.
Expect tougher audits and policy heat as a new report flags Medicare Advantage risk adjustment as wasteful.
Track redeterminations and churn with KFF’s live Medicaid unwinding tracker.
📈 Business & Tech
Free capacity by pointing AI at admin tasks first, not clinicians, says MedCity’s look at workload-lifting AI.
Access to high-cost meds could speed up as Neon Health raises $6M for specialty-drug access tools.
Channel shift watch: Cigna put $3.5B into Shields Health Solutions, reshaping specialty pharmacy.
Grow by pruning outdated habits and standardizing the basics, says AAPC’s revenue potential guide.
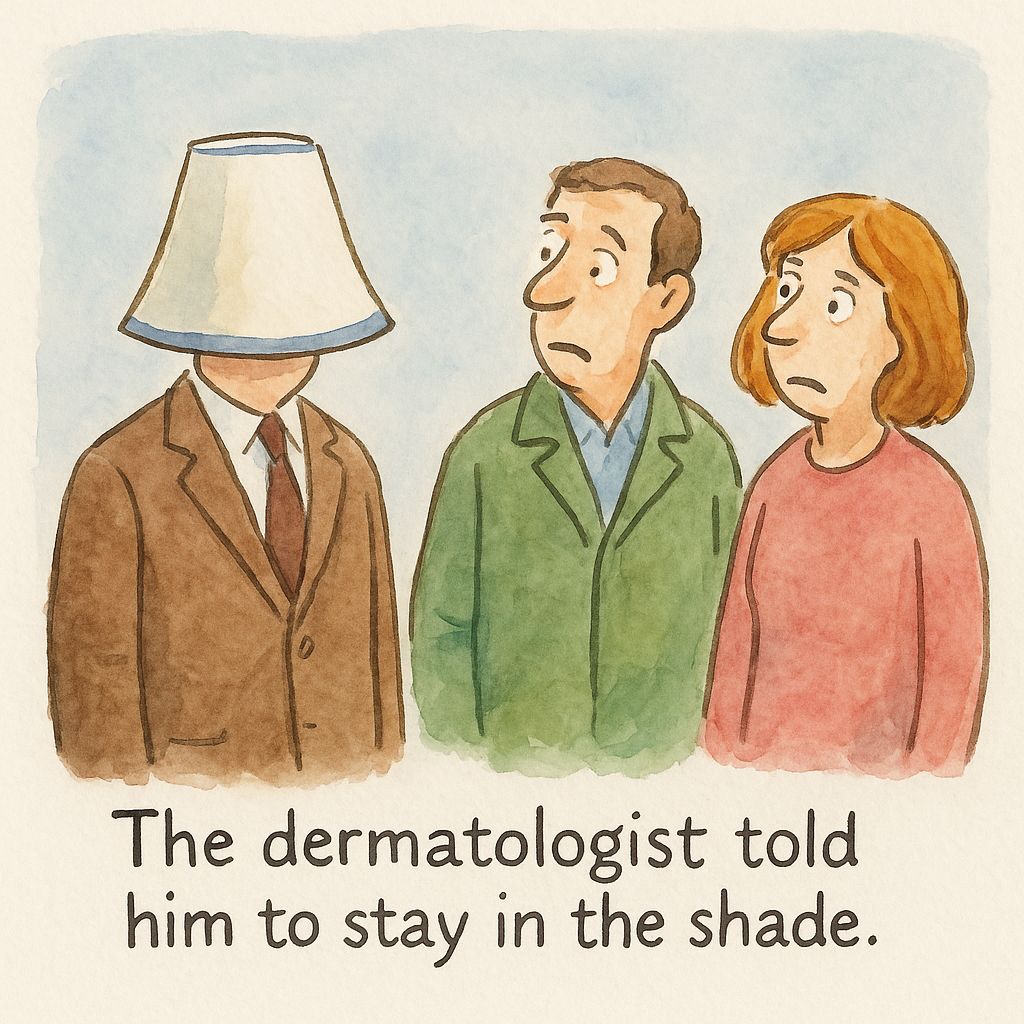
⭐ Just for Fun

The Deep Dive
Getting Paid for Intermediate & Complex Repairs
Complexity doesn’t matter if you don’t document it.
Why it matters: Repairs are routine, medically necessary work in dermatology, but they’re also some of the most commonly denied codes. The culprit? Surprise, surprise: documentation; payers will happily downgrade or deny if your note doesn’t match CPT language. And since CMS clarified the rules in 2020, the bar is clearer (but also higher). If you only do one thing this week, review your templates.
Intermediate (12031–12057): Layered closure of one or more deeper layers, including subcutaneous tissue and superficial (non-muscle) fascia, plus skin. Includes limited undermining, where the undermining distance is less than the maximum defect width, measured perpendicular to the closure line along at least one entire edge of the defect. May also apply to single-layer closure of contaminated wounds after cleaning.
Complex (13100–13153): Meets all intermediate requirements plus at least one of the following:
Exposed bone, cartilage, tendon, or named neurovascular structure
Debridement of wound edges
Extensive undermining (where the undermining distance is equal to or greater than the maximum defect width, measured perpendicular to the closure line along at least one entire edge)
Involvement of free margins (helical rim, vermilion border, nostril rim)
Placement of retention sutures
Restrictions: Excision of benign lesions ≤0.5 cm (11400, 11420, 11440) includes any repair (simple, intermediate, or complex). No separate billing. Keep in mind, this is a Medicare guideline and most commercial payers follow suit.
Payer notes: The core requirements follow CPT. Some commercial plans add documentation nuances or policy language. If denials pop up, check that payer’s policy and align your templates.
Do... | Don’t... |
✅ Document wound length in cm (curved/stellate too). | ❌ Round measurements or leave them out. |
✅ Specify all layers closed, including superficial (non-muscle) fascia, and the suture materials. | ❌ Copy/paste generic “layered closure performed.” |
✅ Record undermining distance and state whether it is less than or at least the maximum defect width measured as defined above. | ❌ Assume “complex” is implied by wound size alone. |
✅ Verify your EHR plan/template captures key requirements. | ❌ Leave quotation marks, placeholders, or fascial layer when not involved. |
✅ Verify note before sign-off. | ❌ Rely on frequent amendments (those flag audits). |
Keep in mind...
Undermining definitions matter: Limited (< wound width) = intermediate; extensive (≥ wound width) = complex.
Excision exceptions: Tiny benign lesions (<0.5 cm) include repair—don’t bill separately.
Template traps: Pre-filled text without measurements is a denial waiting to happen.
⚠️ Documentation Watch-Out: Superficial Fascia
For intermediate repairs, CPT requires layered closure of the subcutaneous tissue and superficial (non-muscle) fascia in addition to epidermis/dermis.
If “superficial fascia” is not named in the note, payers may rule the closure as “skin only” (simple repair).
Simply stating “layered closure performed” isn’t enough.
Best practice: clearly document... “deep subcutaneous tissue, superficial (non-muscle) fascia, and dermis were closed with [suture].”
Why it matters: Even with correct technique, if superficial (non muscle) fascia isn’t explicitly documented, expect denials. Aetna and other large commercial payers are particularly strict here.
Repair Reimbursement Guide
Add EMR templates & fields for undermining measurement, wound width, layers closed, and suture material.
Make sure all providers are trained and know “intermediate = limited, complex = extensive + one more criterion.”
Double-check before signing with a 30-second review. This prevents an amendment (and audit risk).
Quote CPT and payer language in your appeal letters, especially when downgrades hinge on “insufficient documentation.”
Regularly self-audit a random 10–15 repairs and see if documentation matches CPT requirements.
FAQ
Q: Can I bill complex repair if I only do layered closure?
No. Complex requires layered closure plus at least one qualifying element.
Q: Does wound length change classification?
No. Length determines which code within a class you bill, not whether it’s intermediate or complex.
Q: Are repairs bundled with excisions?
Yes, for benign excisions ≤0.5 cm. Otherwise, repair is separately billable if requirements are met.
Q: Can I amend notes after submission?
Yes, but sparingly. CMS requires clear identification of original vs modified content with date and author. Frequent amendments invite audit scrutiny.
Bottom Line: Complexity doesn’t matter if you don’t document it. Miss a measurement or fail to document a required layer, and your intermediate or complex repair can be downgraded or denied. Build templates that force completeness, train your team to use them, and check your notes before signing.
👉 Want to benchmark your denial rate on repairs against other derm groups? Clarity can show you where you stand.

The Toolkit
Things to check out this week
📄 Article You Need: UnitedHealthcare expands its national Gold Card program - more than a 40% increase in qualifying provider groups for 2025; review eligibility and services so you can streamline prior auth.
🛠️ Tool You Should Try: CMS Physician Fee Schedule Look-Up Tool - pull 12031–13153 Medicare rates by locality before you adjust repair templates or negotiate payer rates.
🎧 Event Alert: NCQA Health Innovation Summit 2025 - Oct 13–15, San Diego. Sessions on utilization management, AI risk, and digital quality will help you prep for tougher MA audits.

Need a pro?

When you're ready for an expert to make your practice's billing bulletproof, schedule a strategy call with our team.

That’s it for this week.
This one was super fun. Hope you enjoyed it too.

