Weekly roundup
Here’s what you missed last week!
🏛️ Policy & Payers
Real-time prior auth moves from months to minutes as Highmark Health, AHN, and Abridge pilot ambient AI at the point of care, a signal for faster dermatology approvals.
STRATA Skin Sciences says CPT revisions expand its U.S. addressable market to 30M patients and is pursuing higher reimbursement and competitor litigation.
Nearly 6,500 providers opted out of the $2.8B Blue Cross Blue Shield settlement, underscoring continued antitrust friction with payers.
Medicare telehealth flexibilities face a push for permanent extension from 350+ healthcare groups, preserving virtual access built during the pandemic.
A coming NCPDP standard will touch telehealth, cybersecurity, ePrescribing, data needs, AI, and transparency; practices should expect new tech and workflow asks.
📈 Business & Tech
Infinx’s investment in Maverick AI brings real-time autonomous medical coding to RCM, promising fewer denials and faster cash.
athenahealth rolls out an AI-native athenaOne with “intelligent interoperability,” tightening data flow and reducing clicks for ambulatory teams.
Epic is weaving AI into charting for summaries, notes, and billing support, raising the bar on ambient documentation.
Verrica Pharmaceuticals surprised with profit on YCANTH momentum, a watch item for molluscum treatment access and demand.
Biofrontera reported 15% Q2 revenue growth to $9M on Ameluz sales, even as legal costs widened losses, relevant for PDT supply and promo cadence.
💡 Marketing & Growth
Marchex’s new AI healthcare solution targets patient acquisition and engagement with call insights and attribution dermatology marketers can use now.
Under tighter budgets, health systems are scrutinizing big-ticket marketing deals, doubling down on ROI and goal alignment… good discipline for private practices too.
Sutter Health added 100,000 patients in a year by expanding access, hiring, and leaning on AI-driven digital tools, a blueprint for demand capture.
Five9’s Epic integration promises faster, more personalized patient interactions via contact-center workflows that reduce friction at the front door.
Clutch’s acquisition of Reciprocity Health blends behavioral science with financial incentives to nudge follow-through on care plans and payments.
🩺 Clinical
Teledermatology continues to show strong gains in access and diagnostic efficiency, reinforcing hybrid models for community practices.
Ambient documentation is improving the visit experience as AI scribing reduces screen time and cognitive load for clinicians.
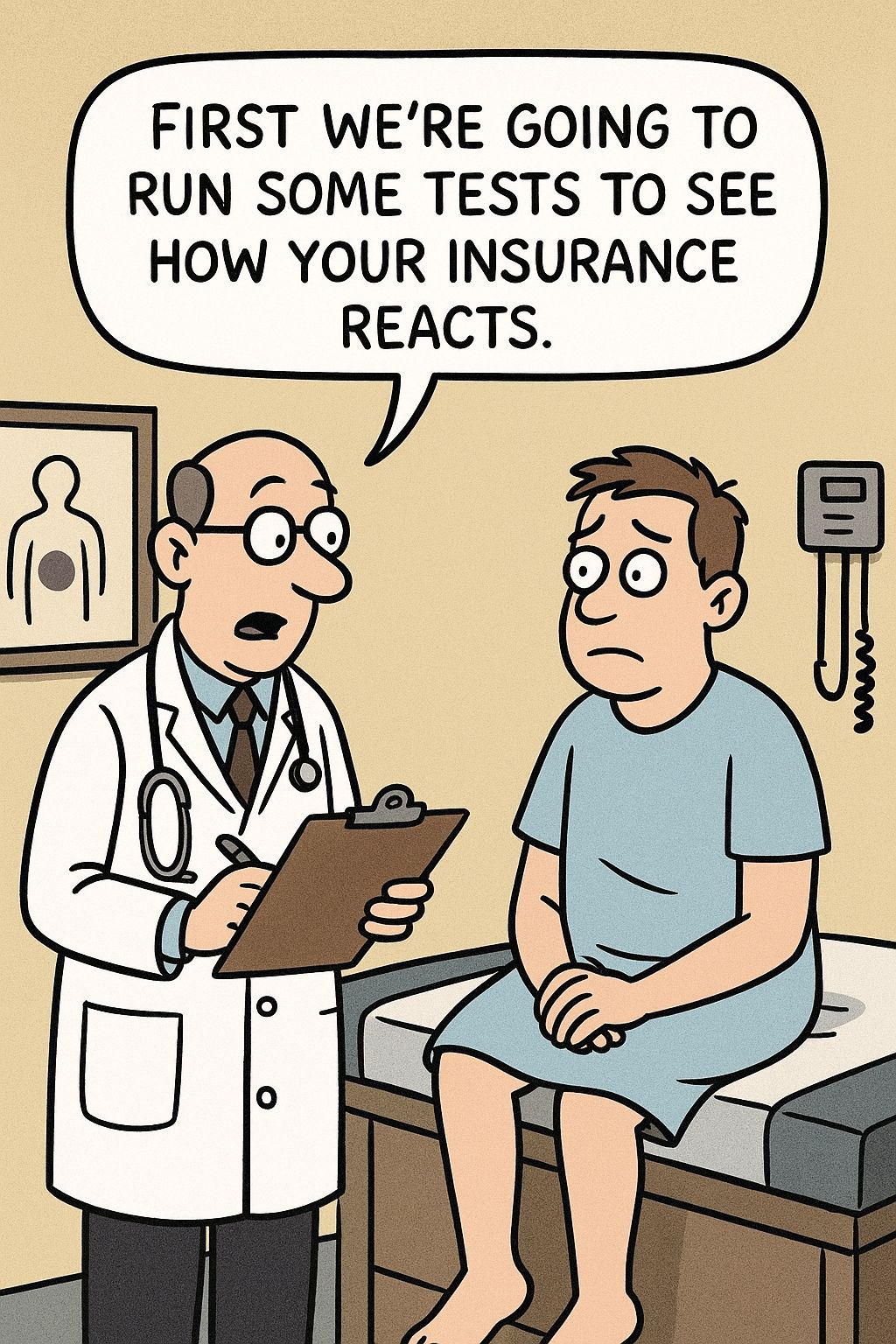
⭐ Just for Fun

The Deep Dive
The New Downcoding Playbook for Dermatology
Do the work once in the chart so you don’t have to do it twice in appeals.
What’s happening? Payers are “right-sizing” high-level E/M claims by auto-adjusting them one level down, often before anyone looks at your note. The AMA has flagged this behavior and states payers should not downcode without reviewing the medical record, yet programs keep expanding.
The new spark. Cigna’s new R49 policy takes effect October 1, 2025. If claim-level criteria don’t support the billed level for 99204–99205, 99214–99215, 99244–99245, Cigna may pay one level lower. If your appeal shows the documentation supports the original level, they’ll restore payment and may later remove you from the program.
It’s not just Cigna. Aetna expanded its Claim & Code Review Program from 12 pilot states to all commercial states except Louisiana in late March, with Medicare Advantage expansion later in 2025. Early removal is possible if you’re able to overturn ~75% of downcoded claims on appeal (keep in mind that even the strongest appeal can fail if the visit note doesn’t support the billed level, which is why provider documentation is the deciding factor).
Anthem BCBS states it began using an analytic solution on Feb 1, 2025 to check whether billed E/M levels align with documentation; selected claims may be denied, pended for records, or paid at a lower level.
MDM vs time. Stay current on how levels are chosen - either MDM or total time. History and exam no longer drive level selection for office/outpatient E/M. For AMA quick guides and tables, see the 2021+ E/M revisions and FAQs.
Medical Decision Making (MDM): the “brainpower” factor. To hit a level by MDM, meet at least two of three elements:
Problems addressed (number/complexity),
Data reviewed/analyzed,
Risk of complications or morbidity/mortality of management.
Time-based E/M: every minute counts. When time determines the level, document total physician/QHP time on the date of the encounter; you do not need to itemize each task minute-by-minute.
Why it matters in dermatology. Evaluation and Management (E/M) visits make up a substantial portion of a dermatologist’s work, alongside procedures. Downcoding directly impacts practice revenue. These programs create a significant administrative burden, as filing appeals is both time-consuming and costly.
Beyond the financial hit, they can delay payment and shift staff attention away from patient care. Advocacy matters here: know your provider representative for escalation, and report downcoding patterns with claim examples to the AAD or other specialty societies. These groups are actively pushing back on inappropriate payer practices and can amplify your voice.
What to look for. Keep an eye out for changes to the billed code, lower-than-expected reimbursement, and vague or missing explanations. Sometimes the amount a payer reimburses for a visit doesn’t seem right. For example, you bill 99214, but the payment matches 99213. When you spot a mismatch, loop in your billing team to investigate. They can review the Electronic Remittance Advice (ERA) to see if the billed code was changed and confirm whether downcoding occurred, then advise on next steps for reconsideration or appeal.
What we’re seeing. Most Clarity RCM clients are not affected, with downcoding shows up in <30% of client sites. Where it appears, it’s highly concentrated: 12 states drive ~91% of volume, led by TX (17%), NJ (13%), PA (8%), VA (8%), TN (8%). Impact varies by practice, from a few scattered downgrades to recurring adjustments. We’re monitoring patterns and pushing back quickly to protect revenue.
Do / Don’t for surviving downcoding
Do... | Don’t... |
✅ Tie level to MDM elements or total time, and say so explicitly in the note. | ❌ Rely on volume of text or templates to imply complexity. |
✅ List each problem addressed, specific tests reviewed/ordered, and risk-driving decisions (e.g., drug toxicity monitoring). | ❌ Use generic diagnoses or omit comorbidities that increase risk. |
✅ Use the most specific ICD-10 codes and link all active problems to the visit. | ❌ Overuse unspecified codes that trigger edits. |
✅ Appeal promptly with highlighted notes mapped to AMA criteria; log win rates to exit programs. | ❌ Accept routine downgrades; it can lock you into a year-long review. |
5-step playbook
Tune documentation now. Make level selection statement (“Level set by MDM: problems+data” or “Level set by total time: 30 min”). Add specific ICD-10 that match complexity and risk; link each problem to the E/M line. This improves appeals and reduces future flags.
Stand up a daily remit check. Compare paid vs contract; move fast before appeal windows close.
Codify appeals. Use a template citing AMA E/M rules and attach the supporting note; for Cigna/Aetna, file reconsiderations quickly.
Measure win rate monthly. if ≥75% with Aetna, request program removal early.
Share deltas with clinicians. Share where appeals fail so note patterns improve.
Gotchas
Time pitfalls: Include only allowable physician/QHP time activities for the date of service.
Program logic: Cigna R49 adjusts a level one step down based on claim criteria, then restores if your records support it.
Bottom line. Downcoding is here, it’s algorithmic, and it’s beatable with precise notes, vigilant remittance review, and disciplined appeals. Do the work once in the chart so you don’t have to do it twice in appeals.

The Toolkit
Things to check out this week

📄 Article You Need: CMS MLN E/M Services Booklet (July 2025) — the Medicare baseline for documentation and level selection, handy for audits and appeals.
🛠️ Tool You Should Try: AMA Downcoding Appeal Letter Template (Word) — prebuilt language to challenge E/M downcoding, ready to customize with your clinical and financial details.
🎧 Event Alert: ONC’s HTI-4 Final Rule info session (recording + slides) — what changes about certification, ePA, and timelines, plus what to ask your vendors next.

Need a pro?

When you're ready for an expert to make your practice's billing bulletproof, schedule a strategy call with our team.

That’s it for this week.
This one was super fun. Hope you enjoyed it too.

