Weekly roundup
Here’s what you missed last week!
🏛️ Policy & Payers
BCBS Michigan will cut E/M reimbursement 50% on same-day services billed with modifier 25 starting May 1.
One in 5 commercial health insurance claims in Massachusetts were denied in 2024, with most rejections tied to administrative errors.
After nearly 20 years of delays, CMS says Medicare Advantage overpayment recoveries targeting $17B in annual overpayments will begin soon.
If a patient presents with symptoms, the resulting test is diagnostic, not a screening, and billing it wrong affects your reimbursement.
Prior authorization requests for Medicare Advantage rose to 53 million in 2024, with nearly 8% denied.
📈 Business & Tech
The dermatology market is projected to grow from $1.41B to $2.75B by 2034, driven by teledermatology and digital health adoption.
AI-powered billing tools are targeting healthcare's $25.7B in billing errors, with early adopters reporting faster clean claim turnaround and less rework.
CommonSpirit is paying Tenet $1.9B to exit its revenue cycle outsourcing contract, betting it can do billing better in-house.
Optum launched two AI-powered prior authorization tools aimed at speeding up approvals for providers and payers.
🩺 Clinical
Dermatologists are seeing growing demand to treat aesthetic side effects of GLP-1 medications, including facial fat loss and skin changes.
AMA added 28 new Category III CPT codes for emerging technologies and revised 4 existing codes.
A new study shows 10-minute pembrolizumab infusions are as safe as the standard 30-minute protocol, freeing up chair time for cancer treatment practices.
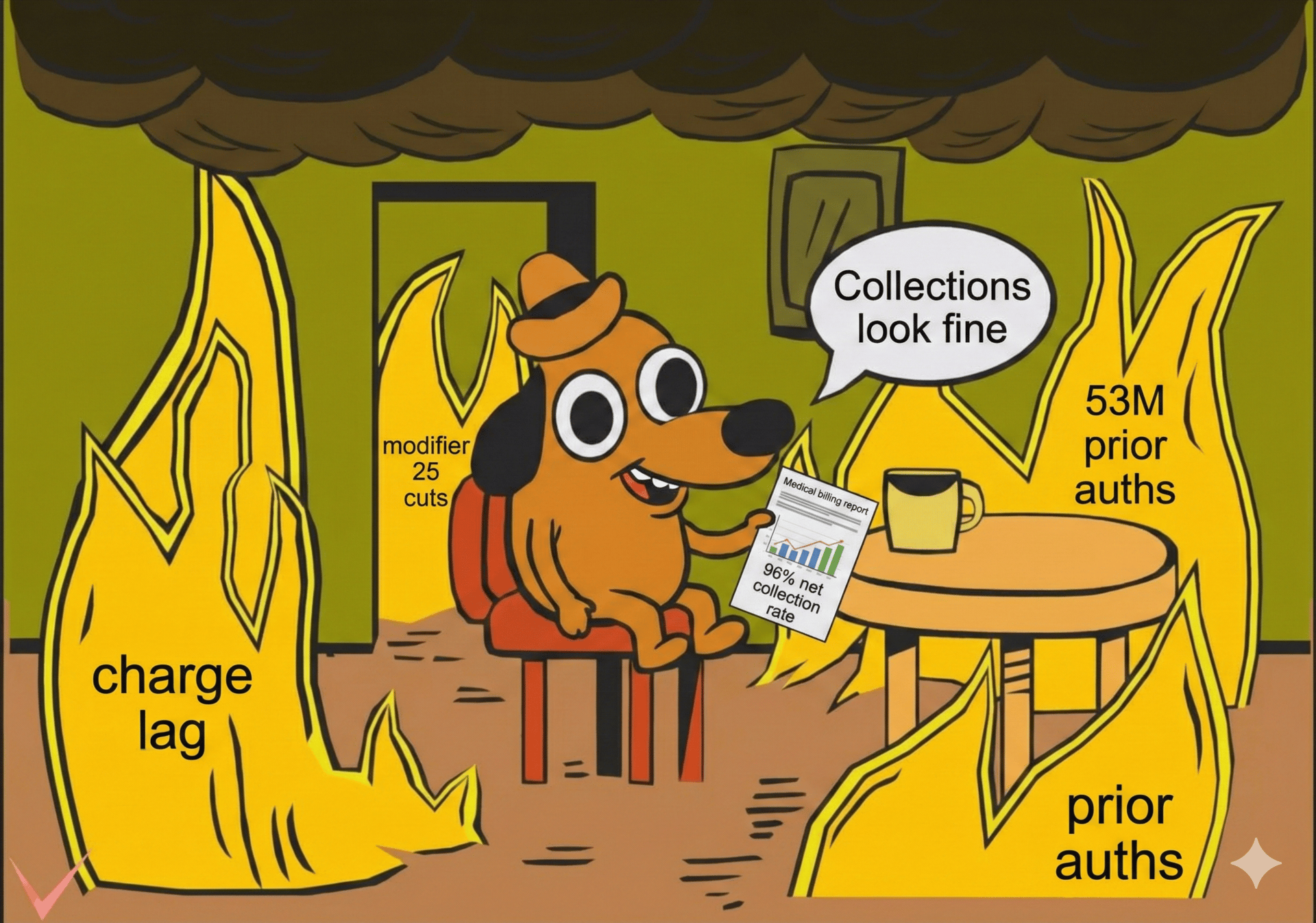
⭐ Just for Fun

The Deep Dive
Collections look fine. These 4 metrics say otherwise.
Your collections report can look perfectly healthy while problems build underneath. By the time those problems show up in collections, they've usually been in motion for weeks.
The earliest warning signs don't live in your collection rate. They live upstream. We’re breaking down the four that matter most:
Charge lag
First-pass clean claim rate
Touchpoints per claim
AR Aging
The metrics that actually predict cash flow
1. Charge lag
Charge lag measures the gap between a patient encounter and claim submission. MGMA benchmarks show charge posting across specialty practices stretching up to 72 hours. For dermatology, where cash flow depends on thousands of small, fast-moving claims, that's too slow.
High-performing practices submit charges within 24 hours of documentation being finalized. That keeps momentum when details are fresh and issues are easiest to fix.
2. First-pass clean claim rate
This is the percentage of claims paid on initial submission without rework. HFMA's MAP Keys set the industry benchmark at 95%. Top-performing derm practices hit 98%.
The gap matters more than it looks. Reworking a single denied claim costs roughly $25. For a practice submitting thousands of claims per year, even a few percentage points of first-pass failure burns real staff hours and real dollars.
And clean claims are only half the equation. Payers increasingly downcode and bundle automatically. Disciplined appeals are what it takes to get the reimbursement you're owed.
3. Touchpoints per claim
In reactive billing environments, claims bounce back and forth. Staff correct errors that should have been caught upstream. Statements go out wrong. Patients call confused.
When eligibility checks, modifier validation, and statement generation happen automatically, billing teams stop firefighting and start focusing on exceptions that require real expertise.
4. AR aging
Total AR tells you how much is outstanding. AR aging tells you whether your revenue cycle is working.
Industry benchmarks place Days in AR for independent practices at 30 to 40 days. High performers average 23 days. On the tail end, industry guidance recommends keeping AR over 90 days below 15%. The best derm practices keep that bucket around 7%.
When AR aging trends the wrong direction, the root cause almost always lives earlier: charge lag, claim quality, or manual workflows creating drag.
What this looks like in practice
A five-provider group came in with a 12 to 15 day charge lag. Charts were finalized in batches. Billing couldn't post until batches closed, so cash flow was inconsistent and the 90+ AR bucket was growing.
After shifting to daily charge capture, setting a 24-hour chart completion standard, and automating eligibility and modifier checks: charge lag dropped below 24 hours. First-pass clean claims went from 84% to 96%. And 90+ day AR was cut nearly in half.
Every metric improved. But the fix started with one change upstream.
Takeaways
Track charge lag weekly. If charts aren't closing within 24 hours of the visit, that delay is rippling through your entire revenue cycle. Set a daily completion expectation and monitor it.
Know your first-pass rate, not just your NCR. Net collection rate tells you what happened. First-pass clean claim rate tells you what's about to happen. If you're below 95%, your scrub rules need attention.
Watch AR aging by bucket, not just total. A stable total AR number can hide a growing 90+ day problem. If that bucket is above 10%, the issue likely started with charge lag or claim quality.
Bottom line: Revenue problems in dermatology rarely start at collections. They start weeks earlier, in the gaps between the visit and the claim. These four metrics show you where.
Clarity helps dermatology practices track upstream metrics and turn them into repeatable workflows. To see what this looks like for your practice, connect with our team.

Need a pro?

When you're ready for an expert to make your practice's billing bulletproof, schedule a strategy call with our team.

That’s it for this week.
This one was super fun. Hope you enjoyed it too.


